NPR Asked All 50 States About Their Contact Tracing Capacity. Here’s What We Learned
BY SELENA SIMMONS-DUFFIN
States are eager to open up and get people back to work, but how do they do that without risking new coronavirus flare-ups? Public health leaders widely agree that communities need to ramp up capacity to test, trace and isolate. The idea behind this public health mantra is simple: Keep the virus in check by having teams of public health workers — epidemiologists, nurses, trained citizens — identify new positive cases, track down their contacts and help both the sick person and those who were exposed isolate themselves.
This is the strategy that has been proven to work in other countries, including China, South Korea and Germany. For it to work in the U.S., states and local communities will need ample testing and they’ll need to expand their public health workforce. By a lot.
An influential group of former government officials released a letter Monday calling for a contact tracing workforce of 180,000. Other estimates of how many contact tracers are needed range from 100,000 to 300,000.
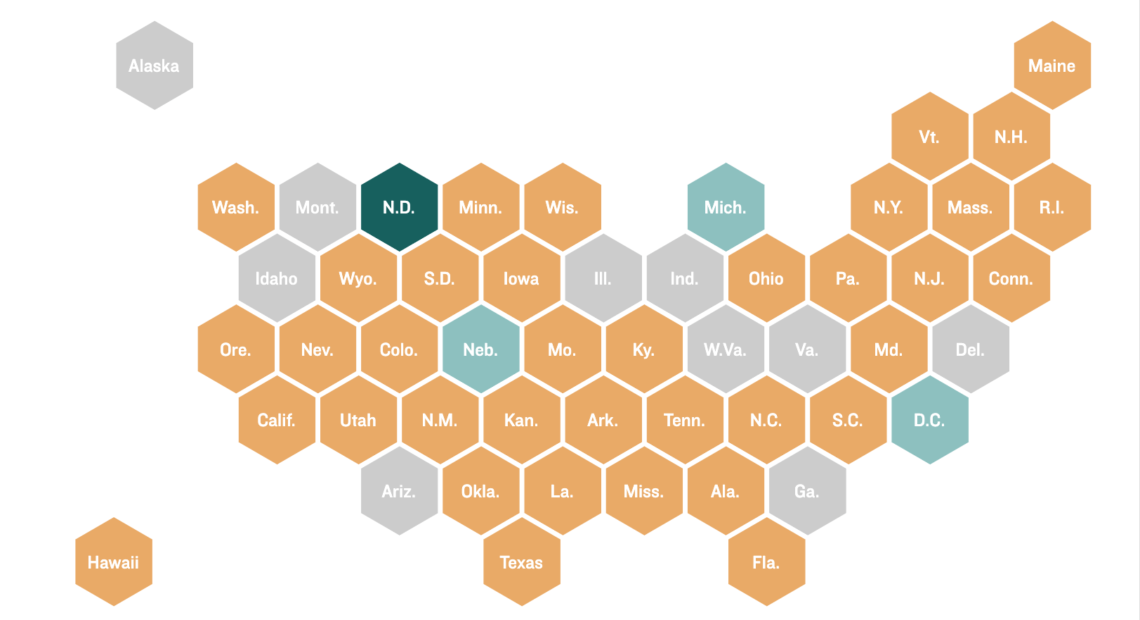
NPR surveyed all 50 states, Puerto Rico and the District of Columbia to ask them how many contact tracers they currently have — and how many they were planning to add, if any. We got data for 41 states and the District of Columbia and found they have approximately 7,324 workers who do contact tracing on staff now, with plans to surge to a total of 35,582.
“It’s a start,” Tom Frieden, former director of the Centers for Disease Control and Prevention, says of these totals. “There are some states that are really thinking about this and scaling it up; there are others that are just beginning to think about it.”
The raw numbers each state needs vary by population size, the number of positive cases, and whether measures such as social distancing have effectively limited the contacts for each case, Frieden says. According to the National Association of County and City Health Officials, which recently issued a position statement on contact tracing, 15 health workers per 100,000 people is a baseline number during normal times, and during a pandemic, this number should double to 30 per 100,000 people.
“That’s probably a good guidepost for state and local health officials,” says Crystal Watson, a senior scholar at the Johns Hopkins Center for Health Security and a lead author of the center’s white paper on contact tracing capacity, though she cautions that these are estimates.
Big hiring efforts, but not everywhere
Several states that took our survey are making big efforts to shore up their contact tracing workforces. Notable examples include Louisiana and Kentucky, which are both planning to hire 700 people; Texas, which has 1,150 contact tracers and is hiring another 2,850 to start; and Kansas, which plans to bring on 400.
“I am really happy to see that there are a lot of places here that are thinking this through, and really putting a lot of effort into that next step,” says Watson. She also notes California’s goal of having 10,000 contact tracers and Ohio’s plan to reach a total of 1,750.
Source: NPR survey of state public health departments, NPR and member station reporting, local media reports, and National Association of County and City Health Officials. CREDIT: Stephanie Adeline/NPR
Of the places that responded to NPR or have released this information in press releases, only four are positioned to surpass that 30 workers per 100,000 threshold: the District of Columbia, Michigan, Nebraska and North Dakota.
In fact, North Dakota stands out dramatically from the pack: After the planned hiring surge it will have 66 contact tracers on staff per 100,000 residents.
“North Dakota leadership believes widespread testing capacity paired with a robust contact tracing infrastructure are key components to rising above this current health challenge,” Vern Dosch, contact tracing administrator for North Dakota, wrote in a statement to NPR. “We are committed to investing in the human resources and technology needed to make it happen. We are building tomorrow on facts, not fear.”
Granted, North Dakota has among the smallest populations of all states — hiring 250 contact tracers to meet the need is certainly easier than onboarding 10,000 in California.
The average rate of contact tracers among the states we had data from was 12 per 100,000 people — just shy of the estimated need during normal times and a third of what’s projected to be needed during the coronavirus pandemic. The median was even fewer: seven contact tracers per 100,000.
Watson warns states against playing this by ear. “This is really something we shouldn’t undershoot,” she says. Of course, public health officials need to keep a close eye on transmission and cases — more cases means you need more contact tracers — but Watson says investing in contact tracing now is the smart move.
“We’re spending trillions of dollars on the economic aspects of this, which is important,” she says. “But if we’re not willing to put in that same effort to the public health side to actually control this and to reduce the economic impacts — fighting this at its source — that doesn’t make sense to me.”
A patchwork of staff and plans in flux
Not every state responded to NPR’s request. A few states – including Idaho and Indiana — did respond, but said they were not able to provide statewide numbers of contact tracers, because contact tracing is done in local health departments. A spokesperson for the Michigan health department explained that state employees assist “certain local health departments with case investigation and contact elicitation, which is the first step in the process of contact tracing,” but the number of county staff that work to trace contacts was not available.
Other states that rely on county health departments to do contact tracing were only able to provide estimates of county staffing levels. Oklahoma’s spokesperson explained that the 150 number of tracers they provided “is a ballpark as we have county nurses who do multiple jobs including contact tracing.”
Another state that was not able to provide contact tracer numbers was Georgia, which has already begun to ease social distancing measures. Spokesperson Nancy Nydam of the Georgia Department of Public Health told NPR that “the total number of contact tracers will vary widely by [health] district, so we are not yet able to put an exact number to it.” She added that the state was engaging with medical students and possibly the National Guard, and that more information would be available in the coming days.
In the survey, several states noted that their plans were very much in flux. “As we are developing our plans, we are hiring and training an initial group of epidemiologists,” a spokesperson for Colorado’s Joint Information Center responded to NPR in the survey, noting they are starting with 50 epidemiologists for now but may add more in the coming weeks.
A few states, including Minnesota, indicated they do not have current plans to hire more contact tracers. Andrea Ahneman, a spokesperson for the COVID-19 Response in Minnesota, wrote that the state had more than 100 staffers now and that “this is plenty of capacity for current needs.”
States that said they’re seeking to expand contact tracing capacity are getting creative about finding the workforce. Nevada said it was recruiting volunteers for “a dramatic expansion” of its contact tracing capacity. Oklahoma is training fourth-year medical residents to do contact tracing. Maine has recruited some recently retired epidemiologists. Georgia and Iowa are planning to call on the National Guard.
About half of states surveyed indicated they were considering the use of smartphone or online apps to assist with contact tracing. Few had decided on a specific app, but several mentioned the Google app that’s in development. Some states indicated that they hoped the federal government could assist with the cost of licensing these apps.
How the federal government can help
Asked what support each state could use from the federal government, several states — including Hawaii, Maine and Nevada — mentioned the need for funding to hire or train new contact tracers. A spokeswoman for the District of Columbia said that D.C. could use “manpower and expertise, especially for training volunteers.”
On the federal level, the Centers for Disease Control and Prevention provides staff to support local contact tracing efforts. Director Robert Redfield told NPR last week that the agency has about 500 staff currently deployed to help state and local health departments, and that it would support another 650 positions with $45 million in funds. He has acknowledged decades of underfunding for public health and said that the federal government needs to “augment personnel substantially.” He also mentioned that his agency is in talks with other agencies and organizations with big boots-on-the-ground workforces to expand capacity, but has not released details on these ideas.
Numerous groups and experts are calling for more action and funds from the federal government. The group of former federal officials who wrote a letter Monday calling for increased contact tracing hires also say $46 billion in federal funding is needed to pay for the hires and resources to help infected and exposed people stay isolated.
Scott Gottlieb, a former Food and Drug Administration chief for President Trump, told NPR on Monday that although assembling as many as 180,000 contact tracers nationally may be daunting, it’s doable. “We already see the states making efforts to bring on thousands of new public health workers to do contact tracing,” he said. “We’re going to need this number of people if we want to enter into the fall with the kinds of resources we need to try to trace infection to prevent large outbreaks.”
Federal leadership on contact tracing is important, says Watson of the Center for Health Security. “This is unprecedented — this is not something we’ve done before as a nation,” she says. “It may be hard for some states to even think about how they get started on this, so guidance from the federal level is definitely needed.”
Stephanie Adeline, Martha Bebinger, Natalie Krebs, Nicole Leonard, Aviva Okeson-Haberman, Sebastián Martinez Valdivia, Anh Nguyen, Bonnie Petrie, Paige Pfleger and Carmel Wroth contributed to this report.