
As Meth Use Surges, First Responders Struggle To Help Those In Crisis
PHOTO-Kim has been living at the Epiphany Center, a treatment facility in San Francisco for women struggling with addiction, for the past six months. She says her teddy bear is her only material possession left from her past: “Because everything I had, I’ve lost over and over again.” CREDIT: APRIL DEMBOSKY
BY APRIL DEMBOSKY
Amelia and her roommate had been awake for two days straight. They decided to spray-paint the bathroom hot pink. After that, they laid into building and rebuilding the pens for the nine pit bull puppies they were raising in their two-bedroom apartment.
Then the itching started. It felt like pinpricks under the skin of her hands. Amelia was convinced she had scabies, skin lice. She spent hours in front of the mirror checking her skin and picking at her face. She even got a health team to come test the apartment. All they found were a few dust mites.
“At first, with meth, I remember thinking, ‘What’s the big deal?’ ” says Amelia, who asked that we not reveal her last name to protect her family’s privacy. “But when you look at how crazy things got, everything was so out of control. Clearly, it is a big deal.”
While public health officials have focused on the opioid epidemic in recent years, another epidemic has been brewing quietly, but vigorously, behind the scenes. Methamphetamine use is surging in parts of the U.S., particularly the West, leaving first responders and addiction treatment providers struggling to handle a rising need.
Across the country, overdose deaths involving methamphetamine doubled from 2010 to 2014. Admissions to treatment facilities for meth are up 17%. Hospitalizations related to meth jumped by about 245% from 2008 to 2015. And throughout the West and Midwest, 70% of local law enforcement agencies say meth is their biggest drug threat.
But policymakers in Washington, D.C., haven’t kept up, continuing to direct the bulk of funding and attention to opioids, says Steve Shoptaw, an addiction psychologist at UCLA in Los Angeles, where he hears one story after another about meth destroying people’s lives.
“But when you’re in D.C., where people are making decisions about how to deploy resources, those stories are very much muffled by the much louder story about the opioid epidemic,” he says.
Even within drug treatment circles, where you’d think everyone would be on the same side, there’s a divide. Opioid addiction advocates are afraid their efforts to gain acceptance for measures like needle exchange programs and safe injection sites will be threatened if meth advocates demand too much.

The stimulant drug methamphetamine is a white, bitter-tasting crystalline powder that dissolves in water or alcohol and is snorted, injected or smoked.
CREDIT: GETTY IMAGES/SCIENCE SOURCE
“The bottom line is, as Americans, we have just so much tolerance to deal with addiction,” Shoptaw says. “And if the opioid users have taken that tolerance then there’s no more.”
So local lawmakers in San Francisco are trying to get a grip on the toll meth is taking on their city’s public health system on their own. Mayor London Breed recently established a task force to combat the epidemic.
“It’s something we really have to interrupt,” says San Francisco District 8 Supervisor Rafael Mandelman, who will co-chair the task force. “Over time, this does lasting damage to people’s brains. If they do not have an underlying medical condition at the start, by the end, they will.”
Since 2011, emergency room visits related to meth in San Francisco have jumped 600% to 1,965 visits in 2016, the last year for which ER data is available. Admissions to the hospital are up 400% to 193. And at San Francisco General Hospital, of 7,000 annual psychiatric emergency visits last year, 47% were people who were not necessarily mentally ill — they were high on meth.
“They can look so similar to someone that’s experiencing chronic schizophrenia,” says Dr. Anton Nigusse Bland, medical director of psychiatric emergency services at Zuckerberg San Francisco General Hospital. “It’s almost indistinguishable in that moment.”
Someone who has methamphetamine-induced psychosis, he says, “they’re often paranoid, they’re thinking someone might be trying to harm them. Their perceptions are all off.”
For example, someone starts walking into traffic on Sixth Street while shouting and taking off his shirt. A bystander calls 911 and reports a mentally disturbed person, and then the police come and deliver him to Nigusse Bland’s department.
If the person is really agitated, doctors might administer a benzodiazepine to calm down, or even an anti-psychotic. Otherwise, the treatment is just waiting 12 to 16 hours for the meth to wear off. No more psychosis.

Dr. Anton Nigusse Bland, head of psychiatric emergency services at Zuckerberg San Francisco General Hospital. CREDIT: APRIL DEMBOSKY/KQED
“Their thoughts are more organized, they’re able to maintain adequate clothing. They’re eating, they’re communicating,” Nigusse Bland says. “The improvement in the person is rather dramatic because it happens so quickly.”
Trends In Drug Use Come In Waves
For some people recovering from addiction, the memories of meth-induced psychosis are part of what motivates them to stay sober.
For Amelia, the scabies scare is what alerted her mother to her addiction, forcing an intervention. Even though she did not have scabies, the itchy feeling and the fear are vivid, even a year and a half later.
“I still don’t really want to say it out loud that it wasn’t real,” says Amelia, now 33.
For Kim, another woman in recovery, there was one day last year when she says she went wine tasting with a friend in Sonoma. She was high on Xanax and speed.
“I was crazy,” says Kim, 47, who also asked that we not reveal her last name. “Meth causes people to act completely insane.”
She and her friend got in an argument in the car. Kim thought someone was behind them, following them. She was utterly convinced. And she had to get away.
“I jumped out of the car and started running, and I literally ran a mile. I went through water, went up a tree, and I was literally running for my life,” she says. “I literally thought I was being chased.”
Kim was soaking wet when she walked into a woman’s house, woke her from bed and asked for help. When the woman went to call the police, Kim left and found another woman’s empty guest house to sleep in. Kim says she just wanted to get warm.
“But then I woke up and stole her car,” she says.
That’s how Kim ended up in jail, in a residential treatment program in San Francisco, part of the steady rise in people seeking help for meth addiction. Rehab admissions in San Francisco for meth are up 25% since 2015.
The trend in rising stimulant use is nationwide: cocaine on the East Coast, meth on the West Coast, says Dr. Daniel Ciccarone, a professor of medicine and substance use researcher at the University of California, San Francisco.
“It is an epidemic wave that’s coming, that’s already here,” he says. “But it hasn’t fully reached our public consciousness.”
Drug preferences are generational, Ciccarone says. They change with the hairstyles and clothing choices, like bell bottoms or leg warmers. It was heroin in the 1970s, cocaine and crack in the ’80s. Then opiate pills. Then methamphetamine. Then heroin. And now meth again.
“The culture creates this notion of let’s go up, let’s not go down,” Ciccarone says. “New people coming into drug use are saying, ‘Whoa, I don’t really want to do that. I hear it’s deadly; people look really doped up and they’re not that fun to be with. I’m going in a different direction.’ ”
Kim has been with meth through two waves. When she got into speed in the 1990s, she was hanging out with a lot of bikers, going to clubs in San Francisco.
“Now what I see, in any neighborhood, you can find it. It’s not the same as it used to be where it was kind of taboo,” Kim says. “It’s more socially accepted now.”
Dying From Meth
A hint about who is using meth today comes from the data on deaths. Meth is not as lethal as opioids: 47,600 people died of opioid-related overdoses in 2017 compared to 10,333 deaths involving meth. (About half of those involved a mix of meth and opioids.) But the death rate for meth has been rising. Meth-related deaths in San Francisco doubled since 2011 and more than quadrupled nationally. This is another indication that more people are using meth and that today’s supply is very potent, says UCSF’s Ciccarone.
Another hypothesis that experts have come up with to explain the growth in meth-related overdoses is that meth users are aging. Most meth deaths are from brain hemorrhage or a heart attack, which would be unusual for a 20-year-old.
“Because your tissue is so healthy at that age,” says Phillip Coffin, a physician and the director of substance use research at the San Francisco Department of Public Health. “Whereas when you’re 55 years old and using methamphetamine, you might be at higher risk for bursting a vessel and bleeding and dying from that.”
Older adults have higher blood pressure, maybe heart disease, that makes their heart weaker.
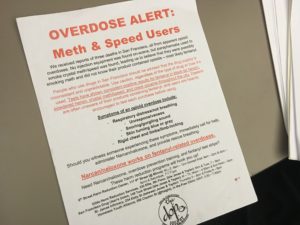
A meth overdose alert from the Drug Overdose Prevention and Education Project. CREDIT: APRIL DEMBOSKY/KQED
“So stimulant-related death, really, you shouldn’t see it affect so many young people,” Coffin says.
The San Francisco AIDS Foundation runs a 12-week program called Positive Reinforcement Opportunity Project to help men who have sex with men stop using meth. The project’s program manager, Rick Andrews, has noticed a trend in older men coming in for help.
“Older gentlemen who grew up in the time of HIV and AIDS initially, maybe they led very safe lifestyles, and now they’re older,” he says.
Now that things are different with HIV — there’s treatment, there’s a prevention pill, PrEP — they’re taking a new approach to the often drug-fueled party scene.
“They feel like they’ve missed out and they want to have a little fun and make up for lost time maybe,” Andrews says.
Another explanation for the rising death rate is that meth is contaminated. And that affects everyone, old and young. Last year, three young people in San Francisco died after smoking meth together. It turns out the meth had fentanyl in it. The synthetic opioid has been causing waves of heroin overdoses across the country, but now it’s showing up mixed into cocaine and meth.
Most researchers believe the contamination is accidental.
“The whole idea of the evil drug pusher who’s trying to create a market by getting their cocaine users hooked on fentanyl — I would highly doubt that,” says UCSF’s Ciccarone.
Dealers know that people are particular about their drugs, he says. It doesn’t make sense to alienate a customer base like that. He compares it to coffee drinkers’ preference for a favorite style of coffee.
“Folks that are doing hardcore illicit drugs can be pretty fussy, too,” he says. “And most meth users really, really, really, really don’t want an unbeknownst fentanyl put into their methamphetamine.”
More likely, Ciccarone says, the same table that was used to cut and bag fentanyl later got used to bag meth.
Deliberate or not, health officials call this poisoning. They started distributing fentanyl test strips to meth users so they can test their drugs. But counselors like Rick Andrews say the strips aren’t refined — even trace amounts will give a positive result.
“I hear guys saying, ‘Oh, there’s test strips and I’m testing. It’s positive, but I do it anyway and everything’s fine,’ ” Andrews says.
That’s why they’re also giving out Narcan, the nasal spray that can reverse an opioid overdose, Andrews says. They’re telling meth users to carry it just in case.
Recovery
Over her two decades of meth use, Kim has been through drug treatment more than a dozen times. Relapse is part of recovery, and among meth users, 60% will start using again within a year of finishing treatment. Unlike opioids, there are no medication treatments for meth addiction, which makes it particularly hard to treat.
Kim finished her last round of treatment in April at a six-month residential program for women in San Francisco called The Epiphany Center. She came to Epiphany directly from jail, after serving time for her housewarming spree and stealing the car. She says in the first 30 days, all she could do was try to clear the chaos from her mind.
“You have to get used to sitting with yourself, which is essential for life, is to get along with your own self,” she says.
Kim is hopeful that this recent treatment will stick. She’s living in transitional housing now, she has a job, and she has been accepted to a program at the University of California, Berkeley to finish her college degree.
“I’ve gone through 12 different programs and it’s been for my children, for my mom, for the courts. I’ve never come to be there for myself,” Kim says. “So it’s like I’ve come to a place where it has to be for me.”
This story is part of NPR’s reporting partnership with KQED and Kaiser Health News.















