Rural Alzheimer’s, dementia patients face disparities in access to care
Listen
(Runtime 1:23)
Read
New research from Washington State University’s Elson S. Floyd College of Medicine shows that patients with Alzheimer’s disease and related dementias who live in rural areas often have to travel much farther to reach neurologists.
That is likely to have a negative impact on patient health outcomes, said Solmaz Amiri, the lead author of the study, because neurologists play an important role in diagnosing neurological disorders like Alzheimer’s Disease and related dementias.
“If people are diagnosed at a later stage, then the cost of treatment will increase over time, and their quality of life will decrease,” she said.
Because there are no statewide registries or datasets on dementia patients and where they live, researchers used mortality data that includes underlying and associated causes of death to determine deceased dementia patients’ distance from their closest neurologist and primary care provider.
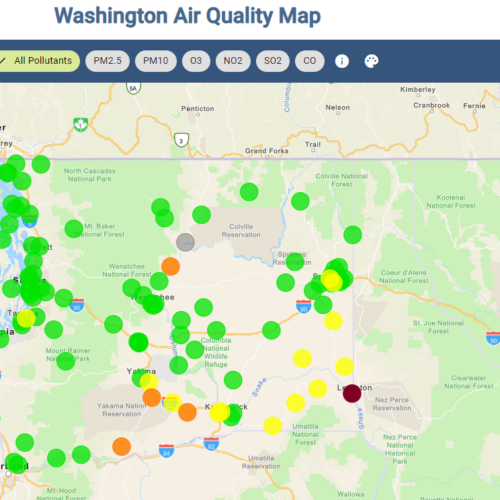
People in small towns and rural areas had to travel an average of 88 and 101 miles, respectively, to reach their nearest neurologist, compared with 9 and 45 miles for metropolitan and “micropolitan” areas, which refers to a city between 10,000 and 50,000 people.
Hispanic, American Indian and Alaska Native populations also tend to have longer driving distances to neurologists because they often live in less urban environments, Amiri said.
On average, Native populations had to travel 28 miles, and Hispanic populations had to travel 22 miles. By comparison, other racial groups had to travel between 7 and 17 miles.
“If we look within Washington state, a large portion of Hispanics tend to live outside of metropolitan areas,” Amiri said. “The same concept applies to American Indian and Alaska Native populations.”
Doctors have medications they can prescribe to slow down memory loss but it’s harder to help patients if they have more advanced forms of dementia, said Dr. Jean Thomas, a neurologist at St. Joseph Regional Medical Center in Lewiston, Idaho.
“Sometimes I get people that come in and they have late or advanced dementia, and then the cow’s kind of already out of the barn,” she said.
The United States is already facing a physician shortage, Thomas said. That shortage is even more pronounced in neurology, particularly in rural areas, and is going to get worse as more baby boomers age.
This year is also set to see record-breaking retirement numbers, with roughly 11,000 people per day celebrating their 65th birthday through December.
Even when patients don’t face additional challenges such as physical impairments that make travel difficult, Thomas said, just the cost of traveling to a hospital can be cost-prohibitive.
“Many of us might find it hard to believe that some patients, they literally cannot afford the gas to drive from Kamiah to Lewiston,” she said.
One saving grace for rural patients, Thomas said, has been telemedicine. Roughly a third of her appointments are through telemedicine, which makes access significantly easier for many of her patients.
Thomas said programs like the University of Washington’s WWAMI (short for Washington, Wyoming, Alaska, Montana and Idaho) Medical Education program, play an important role in introducing medical students into rural medicine and getting them invested in communities.
“I had a pre-med student from Olympia just two weeks ago, and he wants to go into neurology and he shadowed me,” Thomas said. “He loved our practice, he loved St. Joe’s, he liked this community. I think it’s important people know about the WWAMI program and part of that is to try to get these kids wanting to come back into a rural area.”
While the study highlights the need to increase access to neurologists and primary care providers in rural areas, Amiri said, it’s also important to note that the study looks at what would be the shortest possible distance from a provider.
In some cases, patients may have to travel even farther, especially as many neurologists go into specific subspecialties, Thomas said.
“If you want a subspecialist, you’ve got to go to a medical school,” Thomas said.
In addition to rural health disparities, Amiri also noted that some populations may face delayed diagnosis and treatment, as well as overall worse health outcomes even if they do live near neurologists.
“Black populations and Asians, according to our study, tend to live closer to neurologists,” Amiri said. “But the Black populations are one of the racial groups that have a large incidence of dementia, as well as having worse outcomes.”
Part of that disparity may be related to discrimination that Black patients have historically experienced in health care establishments, she said.
“They may not be approaching the services, should they need those,” she said.