Patty Murray Joins GOP Senate Colleague In Targeting High Health Care Bills, Drug Costs
READ ON
BY RACHEL BLUTH / KAISER HEALTH NEWS
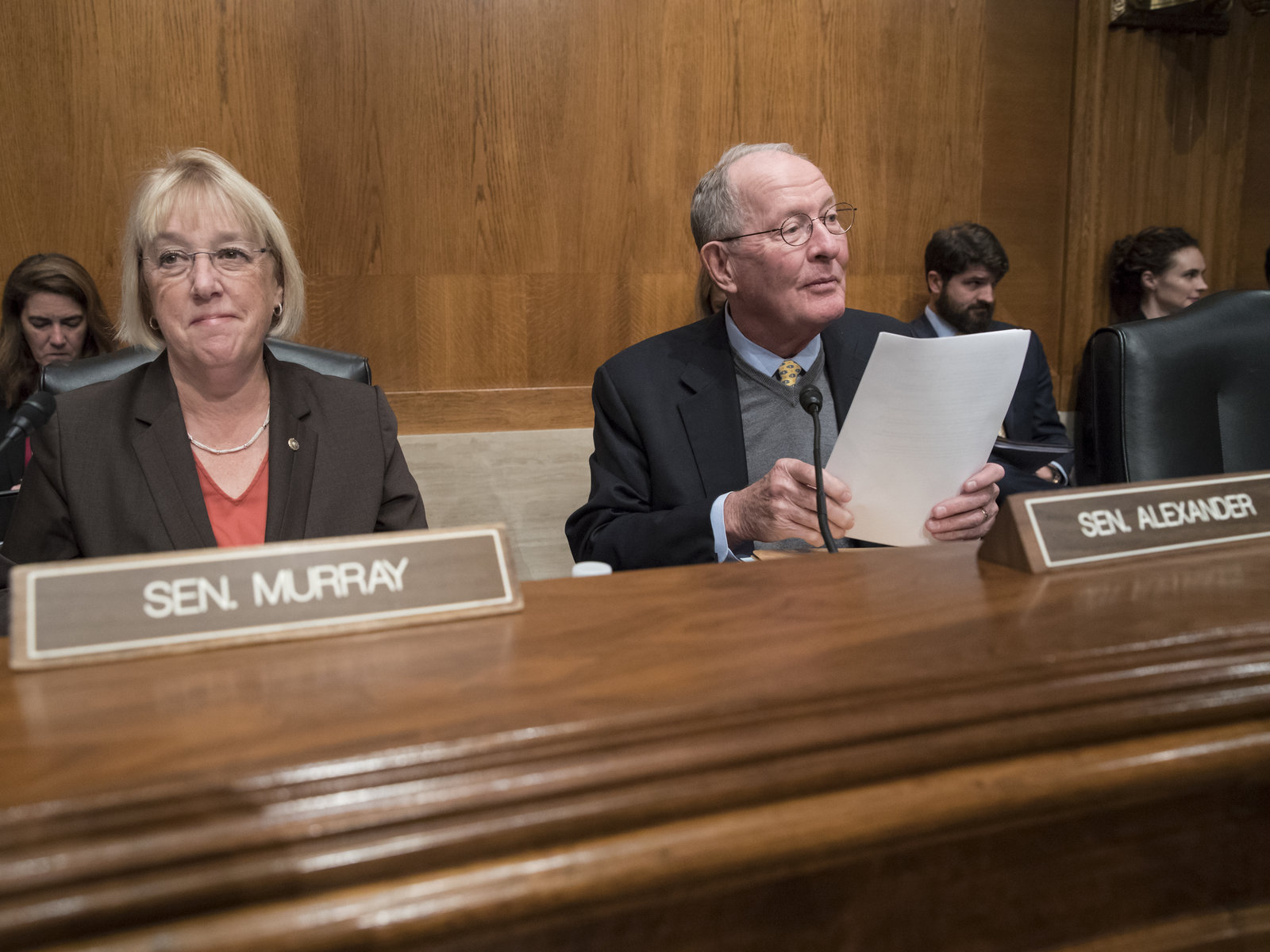
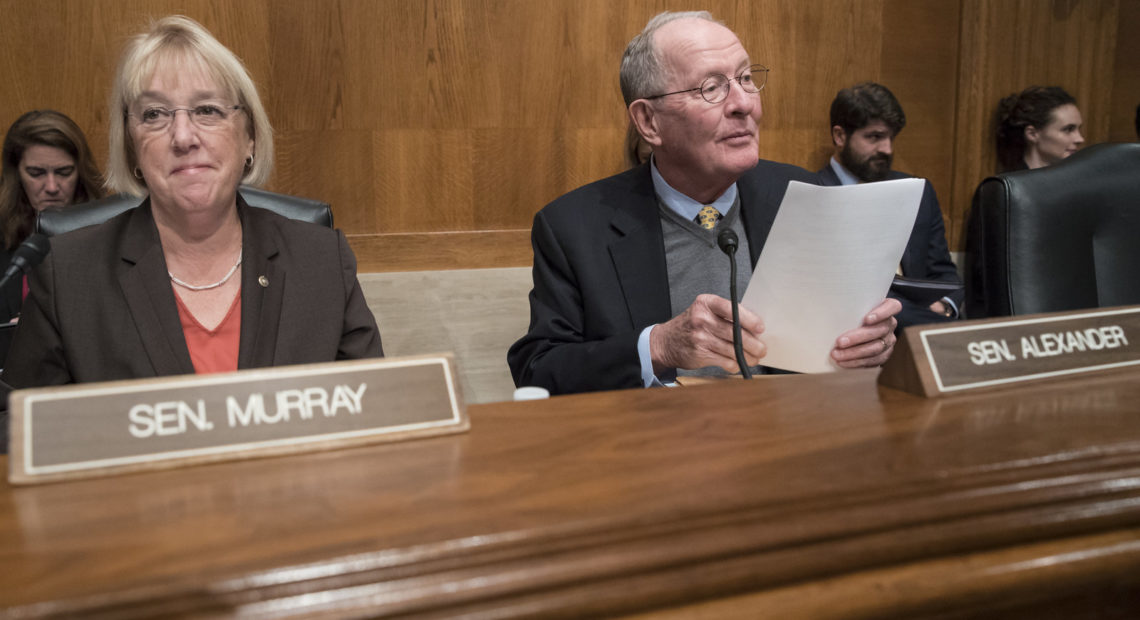
In a year already marked by a wide variety of congressional health care legislation, Sens. Lamar Alexander, R-Tenn., and Patty Murray, D-Wash., on Thursday released the details of a plan they hope will help bring down health costs and eliminate surprise medical bills for patients. Alexander and Murray are the chair and ranking member, respectively, of the Health, Education, Labor and Pensions Committee.
“These are common-sense steps we can take, and every single one of them has the objective of reducing the health care costs that you pay for out of your own pocket,” Alexander said in a statement. “We hope to move it through the health committee in June, put it on the Senate floor in July and make it law.”
It would be a mammoth piece of legislation, targeting nearly every area of the health care industry for reform, including surprise medical bills, prescription drugs, price transparency, public health and health information. Alexander said at a White House event earlier this month that he hopes to get the package to the Senate floor by the end of July.
“When you have a chairman and a ranking member that have worked together on a bipartisan package in the committee of jurisdiction, it always gives more weight to the product,” says Dean Rosen a former Republican senior health adviser and a partner at Mehlman Castagnetti Rosen & Thomas.
“Folks should take this package seriously,” he adds.
The draft bill released by the senators offers three options to curb surprise bills, those unexpected and often pricey bills patients face when they get care from a doctor or hospital that isn’t in their insurance network. It would use an independent arbitrator to settle disputes between insurance plans and providers and set a standard benchmark for physician pay, ideas that have popped up in other draft legislation circulating in the House and Senate.
The novel part from Alexander and Murray is the idea of an “in-network guarantee.” It would require that any hospital considered in-network for a health plan must promise that everyone working there is also in-network.
This would avoid situations in which patients choose a hospital because they know their insurance company will cover the bill, only to find out that one of the doctors they saw was out of network, leaving the patient with a hefty bill.
It also requires that labs and diagnostic tests be in-network, cutting off another avenue of surprise bills.
“From a policy perspective, there’s a rationale that this is the ideal approach,” says Loren Adler, the associate director of USC-Brookings Schaeffer Initiative for Health Policy.
Often called “network matching,” it’s an approach championed by the health insurance industry. James Gelfand, senior vice president for health policy for the ERISA Industry Committee, a trade group representing large employer benefits plans, named it specifically as a solution during testimony at a surprise bill hearing in the House Ways and Means Committee on Tuesday. Rep. Lloyd Doggett, D-Texas, has suggested something similar in bills introduced in this sessions and under the past two Congresses.
It’s possible that this option will upset physicians groups, as doctors risk receiving lower payments and having less leverage with insurance companies. Adler says these fears are mostly unfounded because hospitals have a vested interest in being fully staffed; they’ll step in if insurance companies try to lowball doctors.
Stakeholders such as industry trade groups, lobbyists and consultants will get a chance to air those concerns at a closed briefing on the draft on Capitol Hill on Thursday.
The Alexander-Murray proposal joins an array of efforts on surprise billing. The White House held an event featuring patients, several House committees have held hearings, and bipartisan groups in the House and Senate have proposed legislation, including a bill from Sens. Bill Cassidy, R-La., and Maggie Hassan, D-N.H. In addition to Alexander and Murray’s proposal, the details of another bipartisan bill were released Thursday from Reps. Raul Ruiz, D-Calif., and Phil Roe, R-Tenn., both also physicians.
But Alexander and Murray’s proposal also covers a wide array of issues, and it’s not clear how that will play in Congress just a few months from the start of a presidential election season.
“The steps we are taking on important issues like surprise medical billing, drug prices, maternal mortality, and vaccine hesitancy show we can make progress when both sides are at the table ready to put patients and families first,” said Murray.
“I think it is an ambitious package,” Rosen says. “I think it’s probably going to be a challenge to get all of this done.”
The Alexander-Murray proposal also tackles prescription drug pricing reform, another issue that has raised bipartisan concerns and spurred hearings across the Capitol this spring.
Instead of regulating drug prices, the package would address patent protections, making it easier for generics to get to market and harder for brand-name drugs to maintain exclusive patents for lengthy periods.
It also addresses pharmacy benefit managers, which have lately come under scrutiny in the drug pricing debate. PBMs act as middlemen between drugmakers and insurance plans to negotiate prices and have been blamed by some in the pharmaceutical industry for keeping medication costs high.
The proposal suggests requiring PBMs to give quarterly reports on costs, fees and information about rebates — which are the discounts drugmakers offer to PBMs in exchange for making sure their medication is covered under a health plan. The bill also requires that 100% of these discounts be passed on to consumers.
Other provisions include requiring health plans and providers to give patients estimates of out-of-pocket-costs for a service within 48 hours of a request and mandating that medical bills be sent within 30 days of a procedure.
The bill addresses a host of other health-related issues, including some making headlines recently:
- Money for programs to educate people about vaccines and programs to reduce vaccine-preventable diseases.
- Grants to study and improve maternal mortality and improve pregnancy and postpartum care.
- Money for better training for health care professionals to prevent discrimination and bias.
- Measures to improve privacy and cybersecurity for health information and electronic medical records.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Related Stories:

Idaho doctors say emergency abortion protections are welcome, but not enough
Screenshots of panelists during a press conference on Thursday. Clockwise from top left: Susie Pouliot Keller, chief executive officer of the Idaho Medical Association; Dr. Duncan Harmon, a maternal fetal

CHAS to open additional Lewiston clinic next year
The nonprofit health care provider, CHAS Health, plans to open an additional clinic in Lewiston, Idaho late next year and expand its services.

CAFÉ Pachanga & Mercadito: Wenatchee’s market celebrates Latino culture and health care access for all
Maria Garibay, center, asks Anabella Cardoso, far left, with Esperanza, about social services and health care, while at CAFÉ’s Pachanga & Mercadito resource fair with her son Martin and daughter