
Kaiser: Some small group plans will still have First Fill requirement
Listen
(Runtime 1:26)
Read
Kaiser Permanente’s First Fill requirement in Washington will still apply for Small Group PPO – Summit plans and Virtual Plus plan, according to a statement from Kaiser Permanente. The First Fill program will no longer apply to Large Group base plans, including public and school employees, starting in 2024.
First Fill, which was introduced to Large Group plans in Washington this year, required members to fill maintenance medications through a Kaiser pharmacy or mail-order service after filling their first prescription at a network pharmacy.
The company said some large employers may also still select the First Fill structure for their enrollees as a cost-saving measure.
The program caught a number of enrollees off guard in February. That inspired legislation that would have required insurance providers to give customers a choice in where they fill their prescriptions.
Representative Joe Schmick co-sponsored one of those bills. Though neither it nor its Senate companion made it to a floor hearing, Kaiser Permanente reversed the First Fill decision for 2024.
Schmick said the decision heavily affected his constituents in rural, eastern Washington, where the nearest Kaiser pharmacy is over an hour drive for many residents.
“I just said, ‘What do you have against my small towns that you’re doing this? Because you’re doing this, because you’re killing them,’” Schmick said.
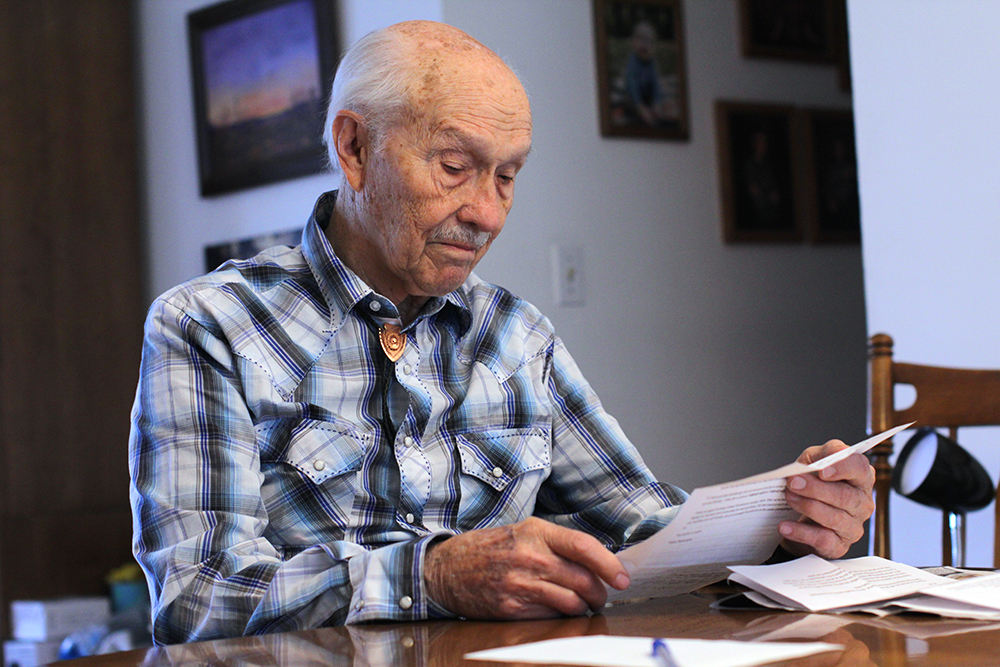
Lee Hadwiger, a retired state employee insured by Kaiser, said he was excited to switch back to his local pharmacy.
“We will probably use Kaiser ‘til we use the present supply of pills, and then go back to [the local] pharmacy after that,” Hadwiger said.
Darcy Linderman is the manager at Sid’s Pharmacy in Pullman, where Hadwiger filled his prescriptions for years before Kaiser enacted its First Fill requirement..
She said the requirement affected about 18% of the pharmacy’s customers. It also required the pharmacy to restructure its staffing, which had been more robust prior to the First Fill requirement.
“We’ve had a number of patients call and say, ‘OK, I’m going to be switching back,’” Linderman said. “It really was a ground-swelling of people taking charge of their rights and saying, ‘I don’t want this.’”
Linderman said the company had already introduced First Fill for some small group plans before it added the requirement to large group plans in Washington this year.
“It’s been a few years for sure,” she said.
Nathan Johnson, the owner of Tick Klock Drug in Colfax, said he still hopes to see legislation pass to limit insurers from adding similar requirements in the future.
“So something like this doesn’t happen in the future with a different insurance company or whatnot,” said Johnson. “But, I mean, I’m happy that things will hopefully go back to normal.”
The requirement made it harder to help patients who were unable to use their insurance if they wanted to keep filling prescriptions locally, or were forced to get prescriptions through the mail, Johnson said.
The legislation Schmick co-sponsored, and its companion, could still pass in the 2024 legislative session due to the legislature’s biennial schedule.
This story was updated to include additional information on Kaiser Permanente Virtual Plus plans also requiring First Fill in 2024.















