Filling Idaho’s health care gaps: Doctors say fixing shortfalls requires more residencies, training programs, continuing education
Listen
(Runtime 1:31)
Read
When Ann Lima goes into work at her clinic, she knows she’ll be treating patients with a range of unique health care needs. She’ll rely on phone calls with specialists and she’ll do her best to stay up-to-date on the broad scope of issues she may encounter.
As a full spectrum health care provider in the small town of Orofino, Lima said, she’s seen an increasing number of people with high medical needs. Idaho has one of the fastest-growing populations in the nation, with many newer residents working remotely. It still ranks lowest in the country in its number of physicians per capita.
That leaves doctors like Lima with a heavy load of patients who have a wide range of medical needs and may not be able to travel for more specialized care. Lima, for her part, does her best to stay on top of as many issues as she can.
“The newest evidence in cardiology and the newest evidence in nephrology, the newest evidence in cardiothoracic surgery,” Lima said. “By no means am I one of those specialists but I am really trying to provide what I’m able to.”
If it seems like a lot for one person, it is. Even with local doctors going above and beyond to provide care, Idaho was ranked last in the country for physicians per capita before the pandemic. Those shortages have worsened since then.
The average age of Idaho doctors is 52, and a 2022 analysis by Idaho Business for Education found about a third of the state’s nurses were expected to retire within a few years.
The state also lost a number of providers this year, including OB/GYNs and the majority of its maternal fetal medicine specialists, following the implementation of strict abortion bans that could result in felony charges for doctors. Physicians, citing fears they could face prison time for providing medically necessary care, left the state.
A May survey by the Idaho Coalition for Safe Reproductive Healthcare found of the 45 OB/GYNs who responded, 51% stated they were considering leaving Idaho, along with 66% of maternal fetal medicine (MFM) specialists.
As of the publication of the survey, only four of the previous seven MFM specialists in the state remained practicing full-time.
To combat the state’s growing health care shortage, one research program is looking at some of the issues facing Idaho’s medical workforce and how to address them. The University of Washington’s multi-state WWAMI program, which stands for Washington, Wyoming, Alaska, Montana and Idaho, runs a research arm out of the University of Idaho, where it also partners to train medical students.
There are three top barriers to Idaho providers’ ability to care for patients, said Russell Baker, associate director of medical research at WWAMI Idaho.
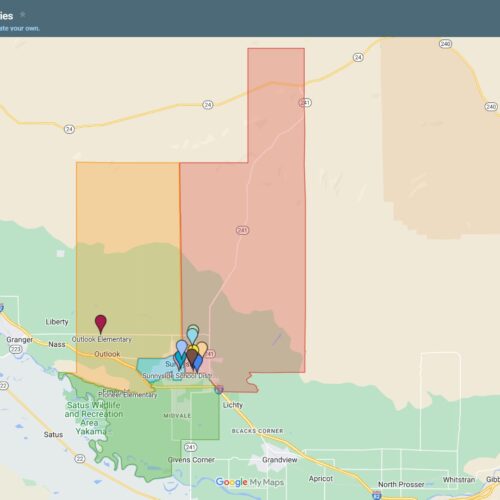
A research project through the WWAMI Rural Underserved Opportunities Program, which connects WWAMI medical students to communities throughout the state, surveyed 445 health care providers from 21 communities on the barriers they faced.
In all seven health districts, doctors identified complexity of patient cases, service access and resource limitations as their greatest challenges. The results were the same in both urban and rural areas.
“So, even the public health districts that had the more urban areas, these are still our challenges,” Baker said. “That’s telling us that, even though you’re theoretically in this urban area, that connectedness to providers is still a challenge.”
The complexity of cases doctors deal with, Baker said, is often worsened when patients delay care because they don’t have a primary care provider.
Access to a primary care provider is generally associated with better health outcomes. Fewer primary care providers means more delayed care, which leads to an increase in complex health issues, Baker said.
Access to a trusted physician can be especially important, he said, for residents in some of Idaho’s communities that may have a higher degree of skepticism about recommended health measures, such as vaccines.
“When we have a situation where you have to be almost forced to do something, in an environment you’re uncomfortable with,” he said. “I’m not surprised that people didn’t follow through with the advised medical care.”
Bolstering Idaho’s medical workforce requires two things, Baker said: Retaining existing providers and training more medical professionals to work in the state.
Some community-wide issues, such as housing prices, can also affect a town’s ability to attract and retain doctors and nurses, Baker said.
“They say things like, ‘I can’t afford to live in this community,’” Baker said. “That just creates greater health disparities and I think that’s one of the reasons we’ve seen migration out of those rural communities of our health care providers.”
Affordable housing and programs to reduce the debt burden on Idaho physicians are two important steps to attracting and retaining providers, Baker said.
Doctors currently practicing in the state also need access to training. One program through WWAMI Idaho, Project ECHO (Extension for Community Health Outcomes). offers training for continuing education in subjects such as buprenorphine administration, a drug intervention for substance use disorder.
Previously, Baker said, physicians were legally required to complete training in order to administer the drug. Even after that requirement was lifted by the federal government, a lack of knowledge still prevented patients from accessing the therapy.
“Our research, pre and post that change, still indicated that one of, if not the top, barrier for providers using that, is lack of confidence or lack of knowledge to provide it,” Baker said. “We can step in and help.”
Providing training to help doctors address the problems they see in their communities could also help the state retain more of its medical workforce, Baker said.
“One of the things that leads people to leave is that they have these challenges and they don’t know how to address them,” he said.
Even with the best training, a limited number of doctors can only do so much. Many of the challenges in providing care circle back to the state’s relatively small number of medical school graduates. In 2022, it was 145 — 41 out of the 47 states — ranked in a list by Becker’s Hospital Review.
Over half of doctors will end up practicing within 100 miles of where they completed their residency (a position for newly graduated doctors to complete required training before being licensed to practice independently).
Similarly, training programs that connect medical students to rural and underserved communities in Idaho can help encourage those students to return when they graduate, said Patrice Burgess, chief medical officer at St. Alphonsus in Boise.
“We’re trying earlier to get students out into the clinical world so they can attach some meaning to what they’re doing,” she said.
Health care providers say training medical students and providing adequate residencies is essential to reducing the provider shortage.
However, those training programs and residencies do have a “chicken or the egg” problem, Burgess said. In order to train students and residents, you need enough doctors to train them and an investment from the state and health care systems in it.
“We need to build up that infrastructure,” she said.
Lima is one of the doctors who works with students and residents from WWAMI, along with medical students from programs in other states, including Minnesota and California.
Bringing students into communities like hers is effective, Lima said, and helps foster a passion for rural health care.
“It brings me joy in not only showing them what real medicine is, but what rural life is, too,” she said.
Even with more providers, fully addressing the state’s health care barriers would also mean addressing social determinants of health that affect patients’ overall wellness and ability to access health care, Lima said.
Some of the biggest barriers her patients face are tied to economic hardship.
“We have such a huge population with unstable housing,” she said. “Always, income is a big issue. We also see a lot of children not getting their needs met.… If I look at the patients that I see on a daily basis, housing, transportation, income are the big ones.”
Many of those challenges were worsened when some patients lost Medicaid coverage this year, after pandemic-era protections that had kept states from disenrolling patients were lifted.
According to the Department of Health and Welfare, around 150,000 Idahoans became ineligible as of April.
For many patients, Lima said, taking care of basic needs would improve their health outcomes.
“More stable housing, and affordable housing, would be huge,” Lima said. “I think housing is probably one of the top things on my list of things that people are lacking.”