
Long-term impacts of Long-COVID among Latinos being researched in WA
Listen
(Runtime 5:08)
Read
Researchers are looking into Long-COVID in Washington. Nearly half of Latinos were asked whether they have experienced prolonged COVID symptoms – and their answers showed they have.
This is part second of a collaborative piece with palabra, the National Association of Hispanic Journalism media outlet, about Long-COVID.
PART ONE: COVID is far from over for some Latinos
In Yakima county, where more people were surveyed, some say there is not much talk about this syndrome.
Doctor Leo Morales is the co-director of the University of Washington Latino Center for Health. He, with another group of researchers, conducted a survey among Latinos to find out if they could be affected by Long-COVID. He presented the results in November in Toppenish – in Washington’s Yakima Valley.
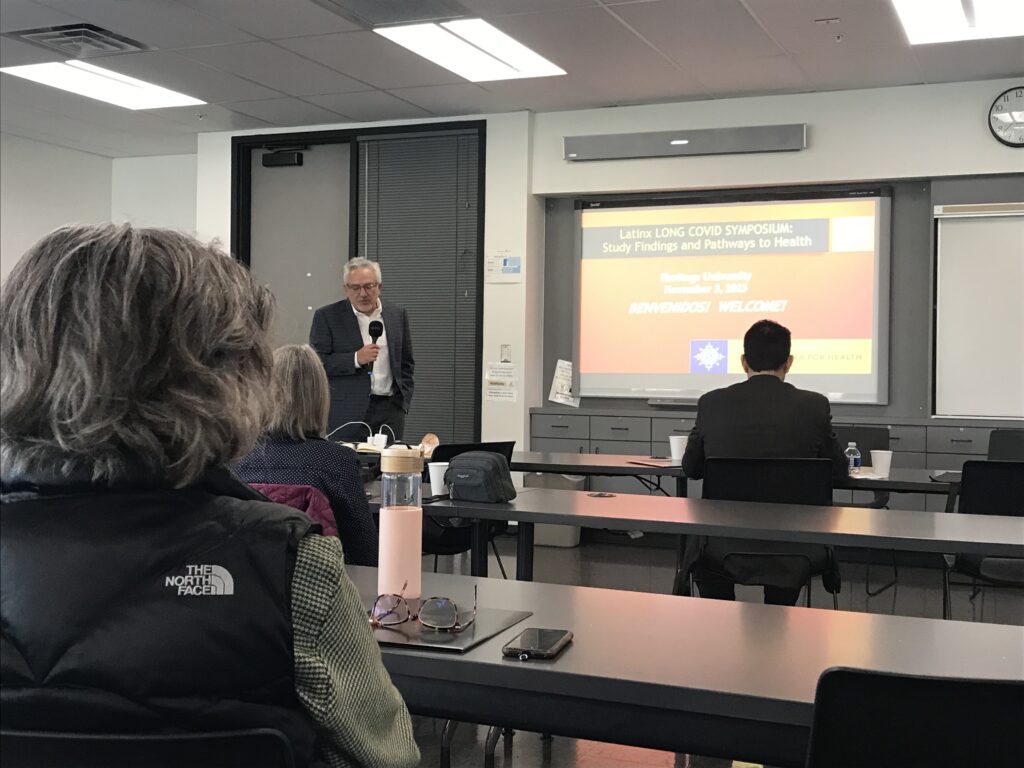
Doctor Leo Morales, co-director of the University of Washington Latino Center for Health, presents the results of the survey on the impact of the Long-COVID on Latinos. (Credit: Johanna Bejarano / NWPB)
“What we found was that around 40% report having new persistent symptoms lasting three months or longer, which means criteria for Long-COVID,” said Morales.
Researchers surveyed Latinos in 19 Washington counties in the west, south center and east areas of Washington. The people were patients of Sea Mar Community Health Centers and Yakima Valley Farmworkers Clinic.
The results show that fatigue, muscle pain, anxiety and sleep difficulty are the top persistent symptoms.
Morales said the data shows that Latinas are more likely to report Long-COVID symptoms.
“This is consistent with other research showing that women are more likely to have Long-COVID than men,” said Morales.
He also said Long-COVID, just like regular COVID, doesn’t affect everybody the same way.
“There’s different patterns of symptoms and it’s probably related to their age and what comorbidities, what other illnesses, they may have,” said Morales.
Doctor Julian Perez is a family physician with Sea Mar Community Health Center in Seattle.
“I see coughs, shortness of breath with work exertion or exercise, headaches, fatigue, body aches that won’t go away, anxiety and depression. Those are the most common presentations I see among my patients and most of my patients are Spanish speaking, Latinos,” said Perez.
Morales said the data is from a significant sample – but researchers are still studying it.
“The data that we shared is based on the people who answered the survey. It’s important to take this as one study and a study with limitations. It’s not everyone in the Latino communities is [are] patients of these two clinics,” he explained.
He said researchers must weigh the data to find more representative findings from the sample.
Perez said Long-COVID is tremendously underdiagnosed.
“We, in the last year, touched 283,000 lives but only 182 diagnoses of Long-COVID were made. What that means to me is that most of the medical providers and behavioral health providers do not identify what people are going through as Long-COVID,” said Perez.
He said that represents a very low percentage of what might actually be going on in the community.
Victoria is a Long-COVID hauler in Sunnyside. She preferred to remain anonymous and not use her real name in this report. She said not everyone understands what she has been going through.
She got COVID, not once but twice, and for months now – said she has dealt with extreme fatigue, brain fog and a chronic cough.
“Visit after visit to the doctor, I would try something for my allergies, it would work for about two months and then the cough came back and I don’t have any proof, because it’s hard to have proof of Long-COVID but I knew it was different,” Victoria said in Spanish.
As a health professional, Victoria said she studied a lot and had to be her own fierce advocate. She said that at this point, Long-COVID is a self-diagnosed syndrome for most.
“It’s self-diagnosis because it’s noticing a change. You must know how you were before and how you are now,” said Victoria.
But not everyone sees these changes, she said, including her parents. She said they have been more tired and dealing with headaches. She said all of that is new, after COVID.
“I tell my dad what that is, and his response is silence. My mom says no, you must rest, all the solutions, but not talking about why we feel that way,” Victoria said.

A local Yakima Valley resident receives the COVID vaccine at a vaccination clinic in Granger, Washington. (Credit: Annie Warren / NWPB)
Antonio Hernandez, a farmworker in the Mabton area, said many haven’t even heard of Long-COVID.
“There have never been any talks, no. No, nothing more than ‘pure sequelae’ of the throat, which are like dryness in their throat. Yes sequelae, but no other diseases, no, I have not heard anything,” said Hernandez.
Hernandez recently attended a COVID vaccination clinic in Granger. For him, getting the vaccine is important. He does not want to get sick again, as happened to him and his wife in 2020.

A sign in front of KDNA, in Granger, advertises COVID vaccination clinic. (Credit: Annie Warren / NWPB)
“She was intubated for seven days. After seven days they checked her well and removed the tubes, because she could breathe well on her own but it was very serious. I spent my time at home alone with home remedies, making hot teas and purely natural remedies but it did look very serious,” said Hernandez.
He also said some of his co-workers were impacted by the pandemic.
“Many people became ill during this period. Many recovered and many died as well,” said Hernandez.
Victoria said, for patients – the hope of getting treatment for Long-COVID depends on having their primary care physician diagnose them. For now, there is little information and even fewer resources in the hard-hit agricultural region of the Yakima Valley in the heart of Washington.
This report is a collaboration between Northwest Public Broadcasting and palabra, the National Association of Hispanic Journalists multimedia platform.
NWPB’s Johanna Bejarano worked with Lygia Navarro, a journalist with palabra. This is the second in the series of collaborative pieces about Long-COVID in Central Washington.

















